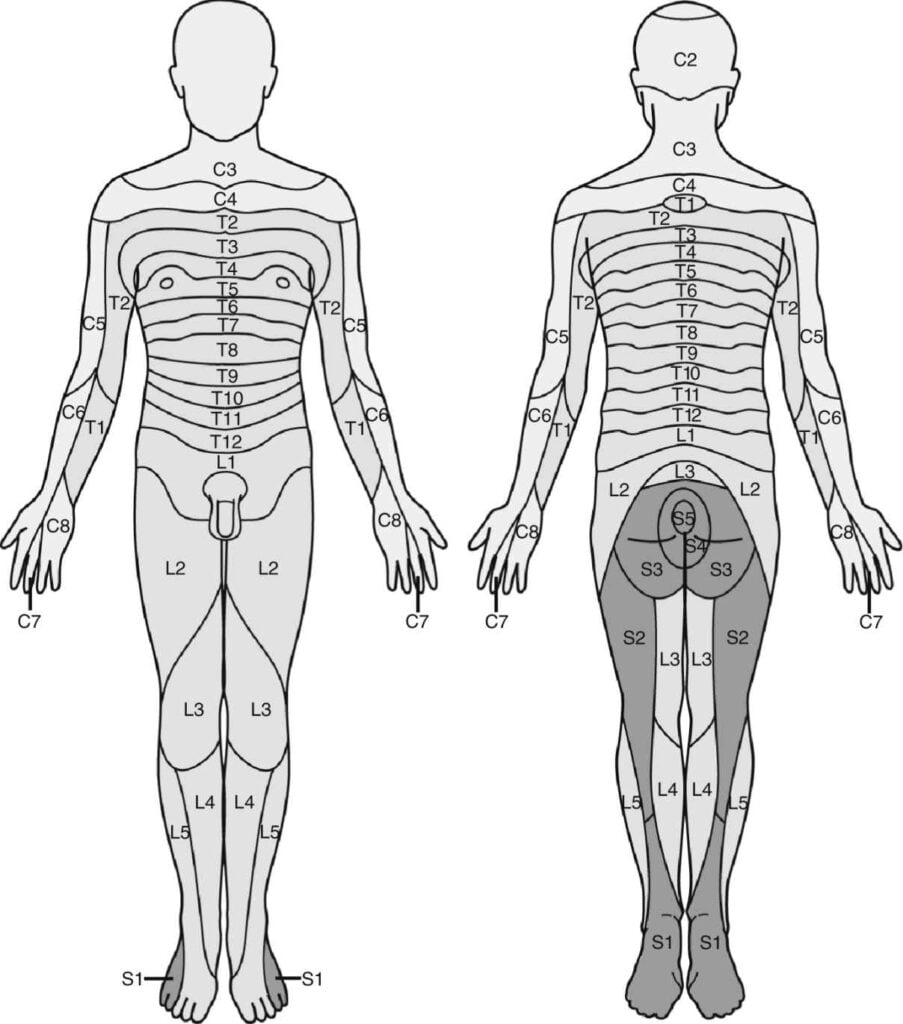
Dermatome Assessment After Spinal Anesthesia – A dermatome is the area of the skin of the human anatomy that is generally provided by branches of a single spine sensory nerve root. These back sensory nerves enter the nerve root at the spine, and their branches reach to the periphery of the body. The sensory nerves in the periphery of the body are a kind of nerve that transmits signals from sensations (for instance, discomfort signs, touch, temperature) to the spine from specific areas of our anatomy.
Why Are Dermatomes Very important?
To understand dermatomes, it is essential to understand the anatomy of the spine. The spine is divided into 31 segments, each with a set (right and left) of posterior and anterior nerve roots. The kinds of nerves in the posterior and anterior roots are various. Anterior nerve roots are accountable for motor signals to the body, and posterior nerve roots get sensory signals like pain or other sensory signs. The posterior and anterior nerve roots combine on each side to form the spine nerves as they exit the vertebral canal (the bones of the spinal column, or foundation).
Regional Anesthesia Anesthesia Key
Regional Anesthesia Anesthesia Key
Dermatome charts
Dermatome maps depict the sensory distribution of each dermatome throughout the body. Clinicians can assess cutaneous experience with a dermatome map as a way to localise lesions within main worried tissue, injury to specific back nerves, and to determine the degree of the injury. Several dermatome maps have actually been developed over the years but are often contrasting. The most frequently used dermatome maps in significant books are the Keegan and Garrett map (1948) which leans towards a developmental interpretation of this concept, and the Foerster map (1933) which correlates much better with medical practice. This short article will evaluate the dermatomes using both maps, recognizing and comparing the major differences in between them.
It’s vital to stress that the existing Dermatome Assessment After Spinal Anesthesia are at best an estimate of the segmental innervation of the skin because the many areas of skin are generally innervated by a minimum of 2 back nerves. If a patient is experiencing pins and needles in just one area, it is unlikely that pins and needles would occur if only one posterior root is impacted due to the fact that of the overlapping segmentation of dermatomes. A minimum of 2 surrounding posterior roots would require to be affected for tingling to happen.
Assessment Guides Dermatomes YouTube
Assessment Guides Dermatomes YouTube
The Dermatome Assessment After Spinal Anesthesia frequently play a significant function in determining where the problem is originating from, offering doctors a tip as to where to check for indications of infection, swelling, or injury. Typical illness that may be partially identified through the dermatome chart include:
- Spinal injury (from a fall, etc.)
- Compression of the spinal cord
- Pressure from a tumor
- A hematoma (pooling blood)
- Slipped or bulging discs
A series of other analysis resources and symptoms are essential for recognizing injuries and illness of the spinal column, including paralysis, bladder dysfunction, and gait disturbance, as well as diagnostic procedures such as imaging (MRI, CT, X-rays looking for bone problem) and blood tests (to check for infection).
Dermatomes play a significant role in our understanding of the human body and can help clients better comprehend how harm to their back can be recognized through numerous signs of pain and other unusual or out-of-place experiences.Dermatome Assessment After Spinal Anesthesia
When the spinal column is harmed, treatments frequently include medication and intervention to lower and combat swelling and rest, inflammation and workout to reduce discomfort and strengthen the surrounding muscles, and in specific cases, surgery to remove bone spurs or pieces, or decompress a nerve root/the spinal cord.Dermatome Assessment After Spinal Anesthesia